What to Expect at Your First Softwave Session
How do I book?
To book your appointment, you can call, text or email our office. Our office staff will find a time and date that works best with your schedule. They will walk you through pricing, our location, and can answer any general questions you may have about treatment or our clinic! Our staff will also send an emailed intake form and consent form your way. It is important that you fill these out sometime before your appointment. Having this basic health history and primary complaint information will help your first time in flow smoothly, while also giving your practitioner the necessary info they need to craft the most ideal treatment plan for you moving forward.
What happens next?
Your Initial session will include some time at the beginning to go through your history, symptoms, concerns and goals. If you’re curious, your practitioner can do a few test shocks on an accessible area, just for you to feel and gauge your comfort level with the feeling. Then the treatment begins!
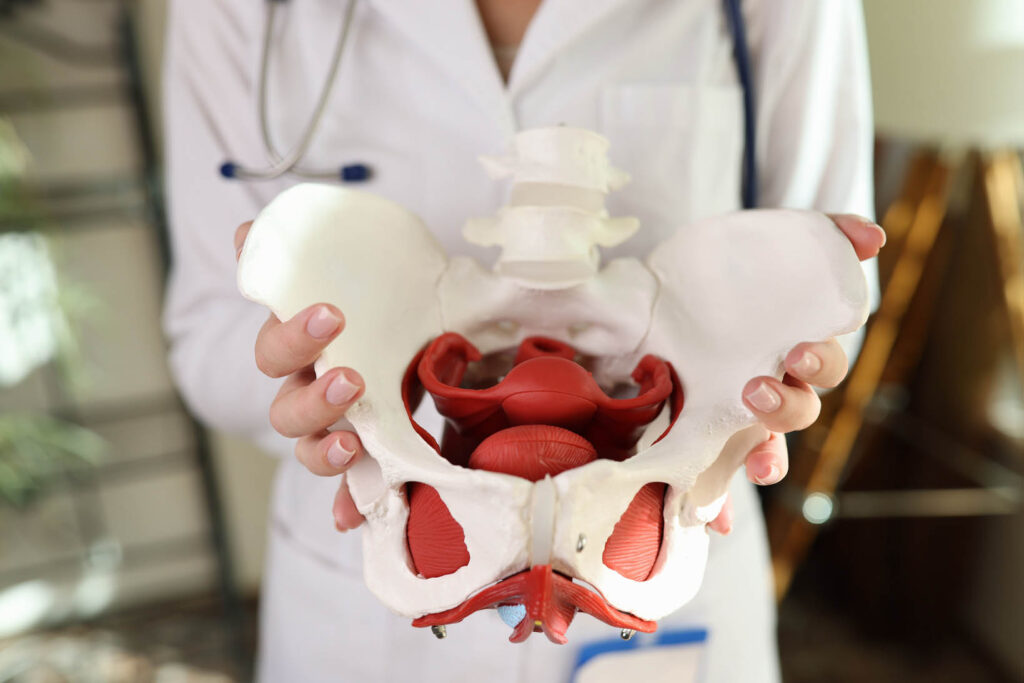
If we’re focusing on pelvic health, or an area of the body that requires an outfit-change, the practitioner will leave the room and give you a moment to undress and cover up with a freshly laundered sheet. If it’s a body part that is a little more accessible, like a wrist or a foot, we will probably dive right into treatment.
An ultrasound gel is applied to the area being treated, and your practitioner will move the applicator around the treatment area as the machine produces the shockwave pulses. Your practitioner will ask you for updates as we move along the tissue- some areas feel a bit like “hot spots”, and we may adjust the intensity of the machine if it feels like too much, or stay on that spot a bit longer, comfort level depending. Either way, you and your practitioner will be in communication the whole time about how things are feeling.
A usual Softwave session at BPHAC is 1500 “shocks” worth of treatment and taking roughly 15 minutes. Erectile Dysfunction treatment sessions are a pinch longer, administering 3000 shocks. At the end of treatment, your practitioner will make sure you know when to book next based on your personalized plan. On your way out, you can cash out and reschedule with the front desk staff, and go about your day as planned!
Immediately After Your Session:
Most people do feel relief after their first session! Sometimes, slight redness or soreness in the treatment area is present. This is normal and usually fades within a few hours to 2 days. It is unlikely, but bruising, swelling, or tingling are also potential side effects. Again, these usually fade within a few hours to a couple days. Feel free to update your practitioner with anything you may notice.
When you return for your follow up session, you and your practitioner will check in about how things are progressing, and administer another session. Staying hydrated throughout the day is always a good idea post any-treatment. You can definitely go about your regular activities, but keep in mind that you may want to give a little extra gentle-ness to the area treated that day.
As progress is made, your time in between appointments will start to space out father apart. Depending on what is being treated, you may be given a rough estimate of time to aim for in between appointments- maybe once a month, or once every 3 months. Some people also come in just as issues arise and flare up, such as injuries from sports.
Regardless of what comes your way, your BPHAC practitioner will be here waiting to help you turn it around!
Book today and feel what this incredible tech can do, especially in the hands of knowledgeable and kind providers. Reach out today!