Beyond the Pelvic Floor: How Acupuncture and Integrative Care Support Healing
Our favorite thing to do at BPHAC? Helping you feel great in your body again!
Our next favorite thing? When our acupuncturists and physical therapists can collaborate on your care, bringing you results from multiple areas of expertise.
Many of our patients benefit from the multidisciplinary nature of our clinic by having an acupuncturist, physical therapist, and massage therapist on our team. We are strong believers in the benefits of having more than one pair of eyes on an issue, and multiple tools in your toolbox.
Combining acupuncture and physical therapy care can be exactly what is needed to address pain, whether something long term & stubborn, or something new that has just reared its head. These approaches combined also work wonders for prenatal and postpartum care; from helping you conceive and maintaining a healthy pregnancy, to preparing for labor/delivery and healing post-birth.
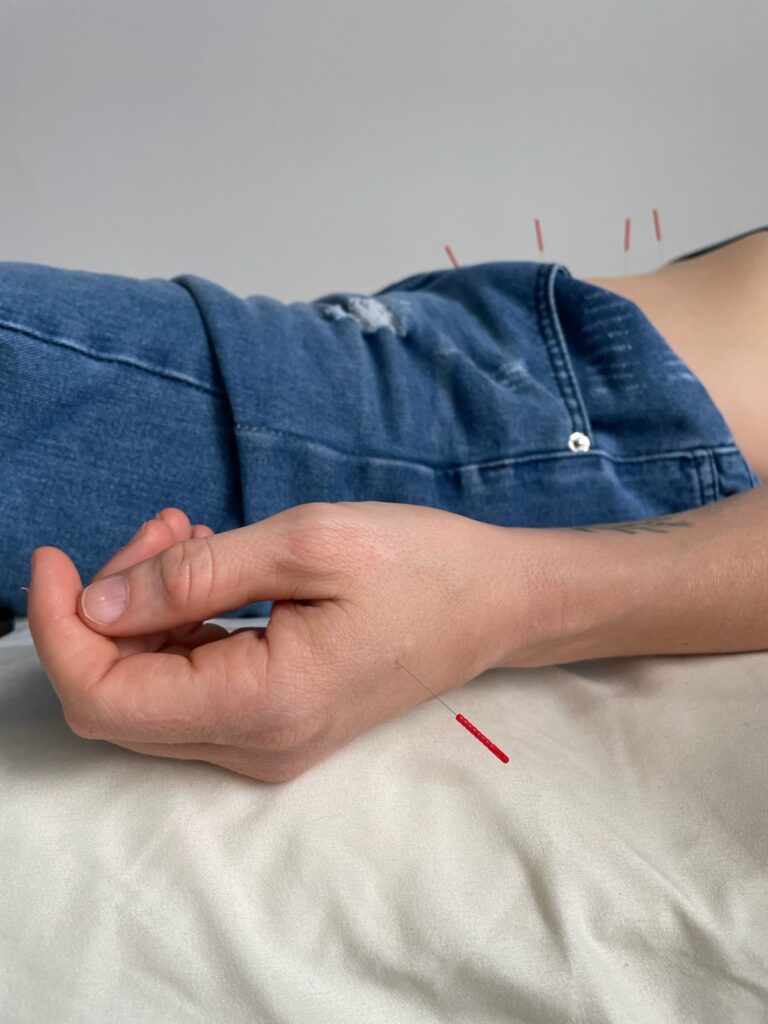
Acupuncture: The Basics
Acupuncture is a traditional Chinese/East Asian medicine practice that involves inserting thin needles into specific points on the body. Traditionally, these points correspond to pathways and meridians in the body through which energy flows. Stimulating certain points along these pathways helps Qi, or the body’s natural energy, to restore and flow properly.
A more modern understanding of acupuncture takes into account the affect that stimulating these points and nerves in the body has a deep affect on the nervous system; bringing the body from “fight or flight” into “rest and digest” which allows the body’s natural healing to occur, while also improving blood flow and circulation, reducing inflammation, and cueing the brain to release endorphins.
While not totally free of sensation, acupuncture does not hurt. In fact, most people fall asleep on the table, and find the experience incredibly calming. The needles are thinner than a strand of hair and very flexible. The initial insertion feels like a fast and gentle pinch, which quickly fades. Acupuncture is safe and side-effect free, making it a great choice for those looking for a more natural way to regulate pain, stress, and improve their health.
Patients usually retain needles on the table anywhere from 30-50 minutes in a session. Additional elements like infrared heat, cupping, moxibustion, gua-sha, or herbs may be included in your session as well. Because acupuncture is a cumulative process, we encourage weekly treatments for your first 3-4 sessions. Some patients see immediate relief, while others need several sessions before feeling lasting results. After your first few, the frequency of sessions usually starts to space out farther apart. The cadence and frequency of treatments necessary will be determined between you and your practitioner, depending on what you are treating and how you are progressing.

Acupuncture & Pelvic Health
For those seeking care for pelvic floor related issues, acupuncture is an incredible option as well. We treat these things together daily in our clinic! Because of its ability to improve blood flow and reduce inflammation, acupuncture can help to get patients out of pain by treating the tissue, nerves, and nervous system, before starting to focus on strengthening and muscle coordination or muscle retraining with a physical therapist.
Acupuncture can help to regulate your body’s nervous system and hormonal health, all of which assists in the treatment of pain, muscle tension, menopause/perimenopause, urinary issues, digestion and constipation issues, pain with penetration and erectile dysfunction, and more.
Acupuncture can help you in your fertility journey, support you through pregnancy pains and morning sickness, help ease anxiety and postpartum depression, and even help flip breech babies and induce labor. Meanwhile, your pelvic floor physical therapist can help ensure you have the exercises, stretches and breathing techniques to ease you into a healthy birth, then help your body heal and strengthen after delivery.

Acupuncture & The Rest of You 🙂
In addition to pelvic health, having an acupuncturist on your team can make a world of difference for your health. Acupuncture can treat virtually every part of the body; so if your pelvic floor pain and incontinence issues resolve, but next you’re hit with seasonal allergies or stress-related headaches, you know exactly who to call next.
Together, your acupuncturist and your physical therapist can help address pain and postural imbalances that may be contributing to your chronic neck, back, and hip discomfort. Not to mention headaches, jaw pain, shoulders, knees and toes, too 🙂
Our practitioners deeply understand how the whole body is interconnected and works together, not as separate parts, and bring that level of understanding to every treatment.

How does this work? What do I book first? Am I seen by both doctors at once?
We require all patients new to our clinic to be seen first for an Initial Assessment. If you’re not sure if acupuncture, physical therapy, or Softwave is the best place to start for you, please reach out to inquire! Our office staff will consult with our providers to try and find the best starting point for you.
If you’re really not sure, oftentimes we highly recommend first coming in for a course of acupuncture treatments. Because acupuncture works internally and so directly with the nervous system, it is an great starting point for a vast array of issues, and has the benefit of being able to treat multiple concerns at once.
If your practitioner at BPHAC refers you to acupuncture or physical therapy to begin working from a different approach, we will set you up with another Initial Assessment to start within this new discipline. The Initial Visit for each unique discipline is an important step in transferring and collaborating on care. It allows your New Doc to have ample time to go through all your history, progress, and goals, while diving into this new aspect of your treatment without being rushed.
Appointments at BPHAC are always 1:1 between you and the practitioner you are seeing. Because each treatment plan is as unique as the individual receiving it, sometimes collaborative care looks like a person alternating back and forth between seeing their acupuncturist and their physical therapist.
It can also look like seeing an acupuncturist for several sessions before switching over to focus on physical therapy for a few visits (or vice versa, of course). It may also just look like your practitioner consulting with one of their colleagues who specializes in another area on your case, with your permission.
Either way, your practitioner will always make use of the fact that at BPHAC, we have the benefit of multiple approaches and specializations under one roof, bringing you the best care possible.